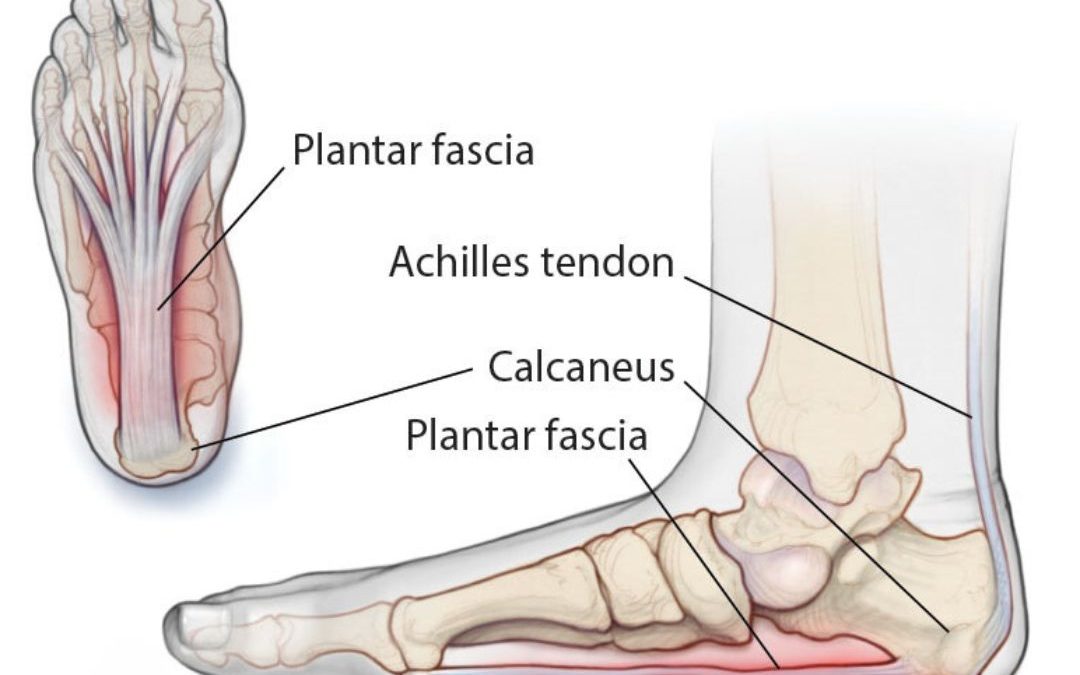
Plantar fasciitis is a common foot condition that causes sharp, stabbing pain in the heel, particularly with the first steps taken in the morning. This condition results from inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of the foot, connecting the heel bone to the toes. Many people suffering from this condition benefit from consulting a plantar fasciitis podiatrist, who specialises in diagnosing and treating foot and ankle conditions to provide effective solutions for managing and relieving the pain associated with plantar fasciitis.
What Causes Plantar Fasciitis?
Plantar fasciitis develops when there is excessive strain or stress on the plantar fascia. This strain can be due to several factors, including:
- Overuse or repetitive strain: Activities that involve repetitive foot strikes, such as running, walking, or jumping, can lead to microtears and inflammation in the plantar fascia.
- Poor footwear: Wearing shoes without proper arch support or cushioning can put extra stress on the heel and the bottom of the foot, contributing to plantar fasciitis.
- Foot mechanics: Abnormal foot mechanics, such as flat feet, high arches, or an abnormal gait, can increase the strain on the plantar fascia.
- Age: The condition is more common in people between the ages of 40 and 60, likely due to the natural wear and tear on the foot over time.
Symptoms and Stages of Plantar Fasciitis
The primary symptom of plantar fasciitis is heel pain, which is often sharp and stabbing, particularly in the morning or after periods of rest. This pain typically occurs with the first steps taken after waking up, making it difficult to walk without discomfort. As the day progresses and the foot muscles warm up, the pain may decrease temporarily. However, it can return after prolonged standing, walking, or engaging in activities that place stress on the feet. The condition can be categorised into different stages based on symptom severity, ranging from mild discomfort to severe, chronic pain that significantly impacts daily activities and mobility
- Recent Onset: In the early stages, patients may experience pain at the base of the heel or a slight pulling sensation in the plantar fascia, which feels like tightness in the sole of the foot. A common symptom in this stage is the sensation of stepping on a stone. This pain typically occurs with the first steps taken after getting out of bed or after long periods of sitting. At this stage, the pain may be intermittent and only mildly uncomfortable, often leading patients to dismiss it as a minor issue. However, early intervention is crucial to prevent progression to chronic heel pain. Simple measures such as rest, icing, and wearing supportive footwear can be effective in managing symptoms and preventing further damage to the plantar fascia.
- Chronic: As the condition progresses, symptoms become more severe and persistent. The pain becomes consistent and more intense, especially in the morning or after periods of inactivity. Walking may become difficult due to the pain, which, although it may ease during the day, can return after extended periods of activity or standing. Patients often feel fatigue and pain later in the day as the foot becomes more stressed, making it challenging to perform everyday tasks. Without proper treatment, the condition can severely limit mobility and negatively impact quality of life.
- Severe: If left untreated, plantar fasciitis can become severe, resulting in debilitating pain that may be constant, even when sitting or lying down. In this stage, patients often have difficulty with daily activities such as walking, standing, or even getting out of bed due to the intense, throbbing pain. The condition can also lead to compensatory changes in gait and posture, which may cause additional strain on other parts of the body, such as the knees, hips, and lower back. In severe cases, the pain can be so intense that it interferes with sleep and significantly reduces the patient’s ability to engage in normal activities. Long-term, untreated plantar fasciitis can lead to chronic pain and may require more aggressive treatments, including corticosteroid injections, physical therapy, or even surgery. Early and appropriate management is essential to avoid reaching this stage and to maintain a good quality of life.
How a Plantar Fasciitis Podiatrist Can Help
Consulting a plantar fasciitis podiatrist is essential for effective management of the condition. A podiatrist offers several benefits:
- Accurate Diagnosis: They will conduct a thorough examination and may use imaging tests, such as X-rays or ultrasound, to confirm the diagnosis and rule out other causes of heel pain.
- Customised Treatment Plan: A podiatrist will develop a treatment plan tailored to your needs, which may include rest, ice, anti-inflammatory medications, and specific exercises to stretch and strengthen the foot muscles.
- Footwear Recommendations and Orthotics: Proper footwear is vital in managing plantar fasciitis. A podiatrist can recommend supportive shoes and custom orthotic inserts to reduce stress on the plantar fascia.
- Advanced Treatments: For cases that do not respond to conservative treatments, a podiatrist may suggest advanced options like corticosteroid injections, shockwave therapy, or minimally invasive surgery.
When to See a Plantar Fasciitis Podiatrist
If you experience persistent heel pain that doesn’t improve with rest or over-the-counter treatments, it’s essential to see a plantar fasciitis podiatrist. Early intervention can prevent the condition from worsening and reduce the risk of chronic pain or further injury. A podiatrist can provide a comprehensive evaluation and recommend effective treatments to help you return to normal activities pain-free.
Plantar fasciitis can be a debilitating condition, but with the help of a plantar fasciitis podiatrist, you can manage and relieve your symptoms. Proper care and guidance from a podiatrist are key to managing plantar fasciitis effectively and returning to your favourite activities without pain.